GENEVA, Switzerland – Since 13 May 2022, cases of monkeypox have been reported to WHO from 12 Member States that are not endemic for monkeypox virus, across three WHO regions. Epidemiological investigations are ongoing, however, reported cases thus far have no established travel links to endemic areas. Based on currently available information, cases have mainly but not exclusively been identified amongst men who have sex with men (MSM) seeking care in primary care and sexual health clinics.
The objective of this Disease Outbreak News is to raise awareness, inform readiness and response efforts, and provide technical guidance for immediate recommended actions.
The situation is evolving and WHO expects there will be more cases of monkeypox identified as surveillance expands in non-endemic countries. Immediate actions focus on informing those who may be most at risk for monkeypox infection with accurate information, in order to stop further spread. Current available evidence suggests that those who are most at risk are those who have had close physical contact with someone with monkeypox, while they are symptomatic. WHO is also working to provide guidance to protect frontline health care providers and other health workers who may be at risk such as cleaners. WHO will be providing more technical recommendations in the coming days.
Description of the outbreak
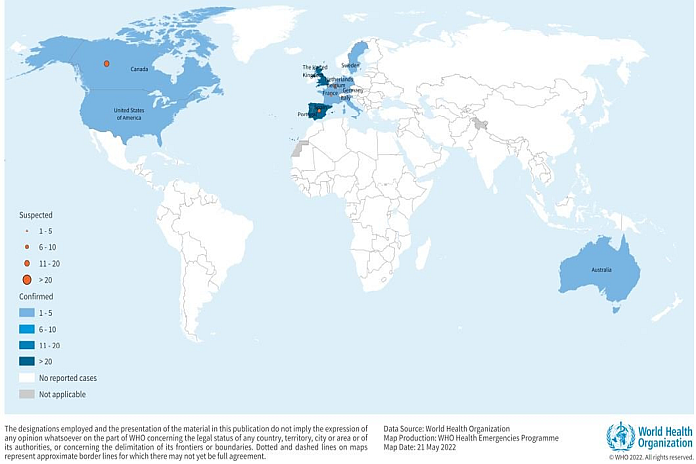
As of 21 May, 13:00, 92 laboratory confirmed cases, and 28 suspected cases of monkeypox with investigations ongoing, have been reported to WHO from 12 Member States that are not endemic for monkeypox virus, across three WHO regions
Reported cases thus far have no established travel links to an endemic area. Based on currently available information, cases have mainly but not exclusively been identified amongst men who have sex with men (MSM) seeking care in primary care and sexual health clinics.
To date, all cases whose samples were confirmed by PCR have been identified as being infected with the West African clade. Genome sequence from a swab sample from a confirmed case in Portugal, indicated a close match of the monkeypox virus causing the current outbreak, to exported cases from Nigeria to the United Kingdom, Israel and Singapore in 2018 and 2019.
The identification of confirmed and suspected cases of monkeypox with no direct travel links to an endemic area represents a highly unusual event. Surveillance to date in non-endemic areas has been limited, but is now expanding. WHO expects that more cases in non-endemic areas will be reported. Available information suggests that human-to-human transmission is occurring among people in close physical contact with cases who are symptomatic.
In addition to this new outbreak, WHO continues to receive updates on the status of ongoing reports of monkeypox cases through established surveillance mechanisms (Integrated Disease Surveillance and Response) for cases in endemic countries as summarized in table 2.
Monkeypox endemic countries are Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Ghana (identified in animals only), Ivory Coast, Liberia, Nigeria, the Republic of the Congo, Sierra Leone, and South Sudan.
Epidemiology of the disease
Monkeypox is a viral zoonosis (a virus transmitted to humans from animals) with symptoms very similar to those seen in the past in smallpox patients, although it is clinically less severe. It is caused by the monkeypox virus which belongs to the orthopoxvirus genus of the Poxviridae family. There are two clades of monkeypox virus: the West African clade and the Congo Basin (Central African) clade. The name monkeypox originates from the initial discovery of the virus in monkeys in a Danish laboratory in 1958. The first human case was identified in a child in the Democratic Republic of the Congo in 1970.
Monkeypox virus is transmitted from one person to another by close contact with lesions, body fluids, respiratory droplets and contaminated materials such as bedding. The incubation period of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days.
Various animal species have been identified as susceptible to the monkeypox virus. Uncertainty remains on the natural history of the monkeypox virus and further studies are needed to identify the exact reservoir(s) and how virus circulation is maintained in nature. Eating inadequately cooked meat and other animal products of infected animals is a possible risk factor.
Monkeypox is usually self-limiting but may be severe in some individuals, such as children, pregnant women or persons with immune suppression due to other health conditions. Human infections with the West African clade appear to cause less severe disease compared to the Congo Basin clade, with a case fatality rate of 3.6 percent compared to 10.6 percent for the Congo Basin clade.
Public health response
- Further public health investigations are ongoing in non-endemic countries that have identified cases, including extensive case finding and contact tracing, laboratory investigation, clinical management and isolation provided with supportive care.
- Genomic sequencing, where available, have been undertaken to determine the monkeypox virus clade(s) in this outbreak.
- Vaccination for monkeypox, where available, is being deployed to manage close contacts, such as health workers. WHO is convening experts to discuss recommendations on vaccination.
Reference tables and further reading is available here.